Strength in Communities: BIPOC Mental Health Awareness Month
- Written by Mental Health America of Eastern Missouri
 Known also as BIPOC Mental Health Awareness Month, Bebe Moore Campbell National Minority Mental Health Awareness Month was created to bring awareness to the unique struggles that underrepresented groups face regarding mental illness in the United States. Campbell was an American author, journalist, teacher, and mental health advocate who worked tirelessly to shed light on the mental health needs of the Black community and other underrepresented groups.
Known also as BIPOC Mental Health Awareness Month, Bebe Moore Campbell National Minority Mental Health Awareness Month was created to bring awareness to the unique struggles that underrepresented groups face regarding mental illness in the United States. Campbell was an American author, journalist, teacher, and mental health advocate who worked tirelessly to shed light on the mental health needs of the Black community and other underrepresented groups.
Over the years, Black, Indigenous, and People of Color (BIPOC) and queer and trans BIPOC (QTBIPOC) communities have developed systems of support to fill the gaps within mainstream healthcare systems. Three main topic areas within these support systems are community care, culturally-based practices, and self-directed care.
Community Care
Community care is an approach utilized by individuals to support one another and the broader community. Community care has existed in BIPOC and QTBIPOC communities for generations as this approach relies on the collectivistic beliefs of many of these communities, where the well-being of the individual is intrinsically tied to the well-being of others, including the larger community. Community care focuses on the connections, intentional actions, and efforts to mobilize individuals to support one another. Community care includes but is not limited to: mutual aid, healing circles, community healing, doulas, faith practices, community health workers, and peer support.
A foundational aspect of community care is the recognition of inequities that exist for individuals and communities. These inequities are often tied to larger systemic barriers and structures often referred to as social determinants of health that directly affect the well-being of individuals, including economic factors, access and quality of education and health care, the physical environment, and other complex community structures. As a result, community care responds to existing inequities and gaps in resources by creating new structures to bridge gaps and to increase access to meaningful resources through mutual support and aid provided by individuals and broader community-focused efforts.
How Community Care Impacts Mental Health
In essence, community care pushes individuals to think about their well-being as an extension of the well-being of the community they are a part of and belong to, thus individuals work collectively and in solidarity with one another to identify and respond to needs that impact communities as whole systems. Community care is also critical to an individual’s mental health as it responds to the isolating factors often experienced by individuals who may feel disconnected to their community due to life circumstances, the impacts of racism, marginalization, violence, trauma, and other societal factors.
Community care enables individuals to find belonging, connection, and collective support in a welcoming environment—factors which are tied to improved recovery from mental health conditions and overall well-being. Additionally, community care allows for individuals to feel valued and taken care of in a mutually respectful manner by members of their community.
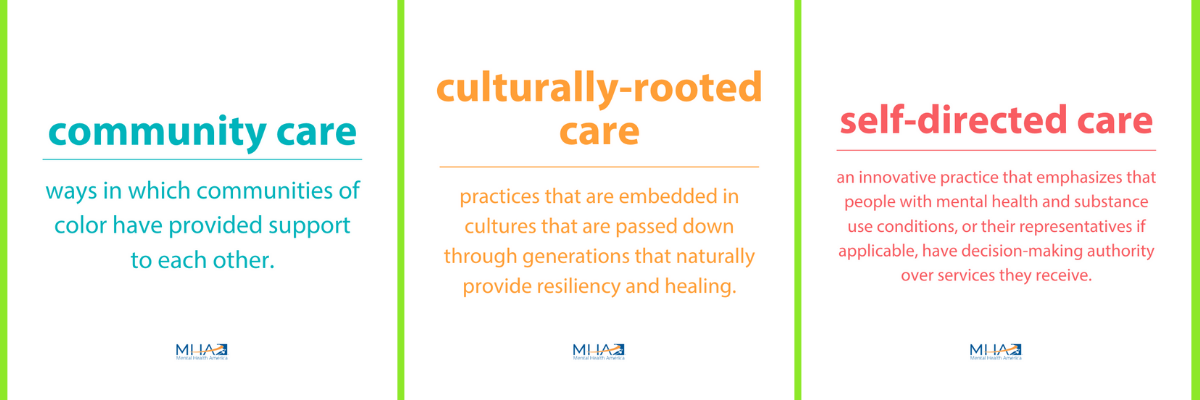
Culturally-based Practices
Culturally-based practices are culturally-rooted customs, behaviors, values, and beliefs passed down through generations that function as “informal systems of support.” These culturally-based practices form part of a socially dynamic framework of assistance provided by and to individuals by their families, friends, and communities. A culturally-based practice relies on intergenerational knowledge sharing of customs, ancestral history and heritage, traditional practices, and relationship structures that function as key elements that provide comfort, security, trust, and healing for the individual and the broader community These culturally-based practices provide a safe space for individuals to talk about and share their lived experiences without the need for explanation or justification of feelings.
Culturally-based practices are so deeply ingrained within an individual and a community that their existence may often go unnoticed as people naturally integrate these practices into their daily life, significant life experiences, or during times of distress and illness. Sometimes, they are very present and intentional - like building an altar - but can also be less visible such as relationships with elders developed through shared activities such as prayer circles.
How Culturally-based Practices Impact Mental Health
For generations, culturally-based practices have been erased, set aside, hidden away, or utilized in secret. The efforts to erase these practices are a cornerstone of the oppressive and violent actions implemented toward diminishing the history, value, and pride in BIPOC and QTBIPOC communities. As a result of these aspects of historical trauma, individuals and communities modified their behaviors to keep themselves and the practices protected.
Unfortunately, the long-term impact of these behavior modifications has often resulted in individuals being unaware of culturally-based practices or hesitant to engage in them out of fear. It is important to shed light on and engage in culturally based practices in order to heal. By embracing culturally-based practices, individuals and communities can begin the process of understanding the impacts of historical trauma, reclaiming the honor and pride of their ancestors, their historical knowledge, and the power that exists in connecting with one’s community through shared values, beliefs, and customs.
Self-directed Care
Self-directed care (SDC) is an innovative practice that emphasizes people with mental health and substance use conditions should have decision-making authority over the services they receive. Individuals are encouraged to take direct responsibility to manage their care, including determining their own needs, deciding how those needs are met, and continuously evaluating the services.
In SDC programs and initiatives, individuals control a budget that supports them in working toward their recovery and wellness goals. These financial resources can be used for things like transportation, gym memberships, employment-related goods and services, and traditional mental health services.
How Self-directed Care Impacts Mental Health
The way people talk about, and experience mental health is uniquely shaped by their racial and ethnic backgrounds and cultural experiences. Because SDC gives the individual seeking services the power to decide what works best for them, it allows people from marginalized communities to determine their own priorities in recovery and move beyond traditional systems of care, which were not originally designed with them in mind.
SDC creates space in treatment plans for culturally relevant services and goes beyond diagnosis to treat the whole person. SDC grants individuals autonomy, agency, and choice. It gives people seeking services the freedom to decide what is meaningful and life-enhancing to them. These factors are crucial in empowering individuals to take control over their own care, wellness, and life - and when people are motivated, they are more likely to succeed in recovery.
Be an Ally
Everyone can take action to support the mental health wellness of BIPOC and QTBIPOC individuals. Whether you identify as a member of these communities or want to be a stronger ally, the following steps help promote mental health and increase access to care.
- Push for accessibility in traditional health care by contacting your local elected officials. Use channels like social media to talk about these issues. Call for expanded language services, culturally responsive provider training, and expanded public education resources around health literacy.
- Hold organizations and institutions accountable. Our health care systems are not the only ones responsible for BIPOC mental health. Ensure that the systems you are a part of, including workplaces, research institutions, schools, and political structures actively assess how they contribute to the problems that exist for BIPOC and QTBIPOC mental health.
- Think beyond traditional health care. When advocating or looking for resources for yourself or a loved one, keep non-traditional health care supports in mind. If you find that the mainstream health care systems do not support BIPOC mental health effectively, expand criteria to include community support that may not come up in traditional searches or doctor recommendations.
- Give credit to originating communities of healing practices. Many BIPOC and QTBIPOC identifying individuals and communities developed their resources and supports to address mental health needs. However, they do not always get credit for these practices if they become adopted by mainstream society. If you choose to utilize a BIPOC-established approach, ensure that you give credit to the originating community and encourage others to do the same.